Test all. Test early. Test for H3 K27M
About H3 K27M
The H3 K27M mutation is associated with poor prognosis in diffuse gliomas1-3
H3 K27M–mutant diffuse gliomas can occur across the brain, in both midline and non-midline structures, and are characterized by the global loss of H3 K27 trimethylation (H3 K27me3 loss).4,5

Non-midline structures
Midline structures
Molecular and cellular changes arising from the H3 K27M mutation4,6
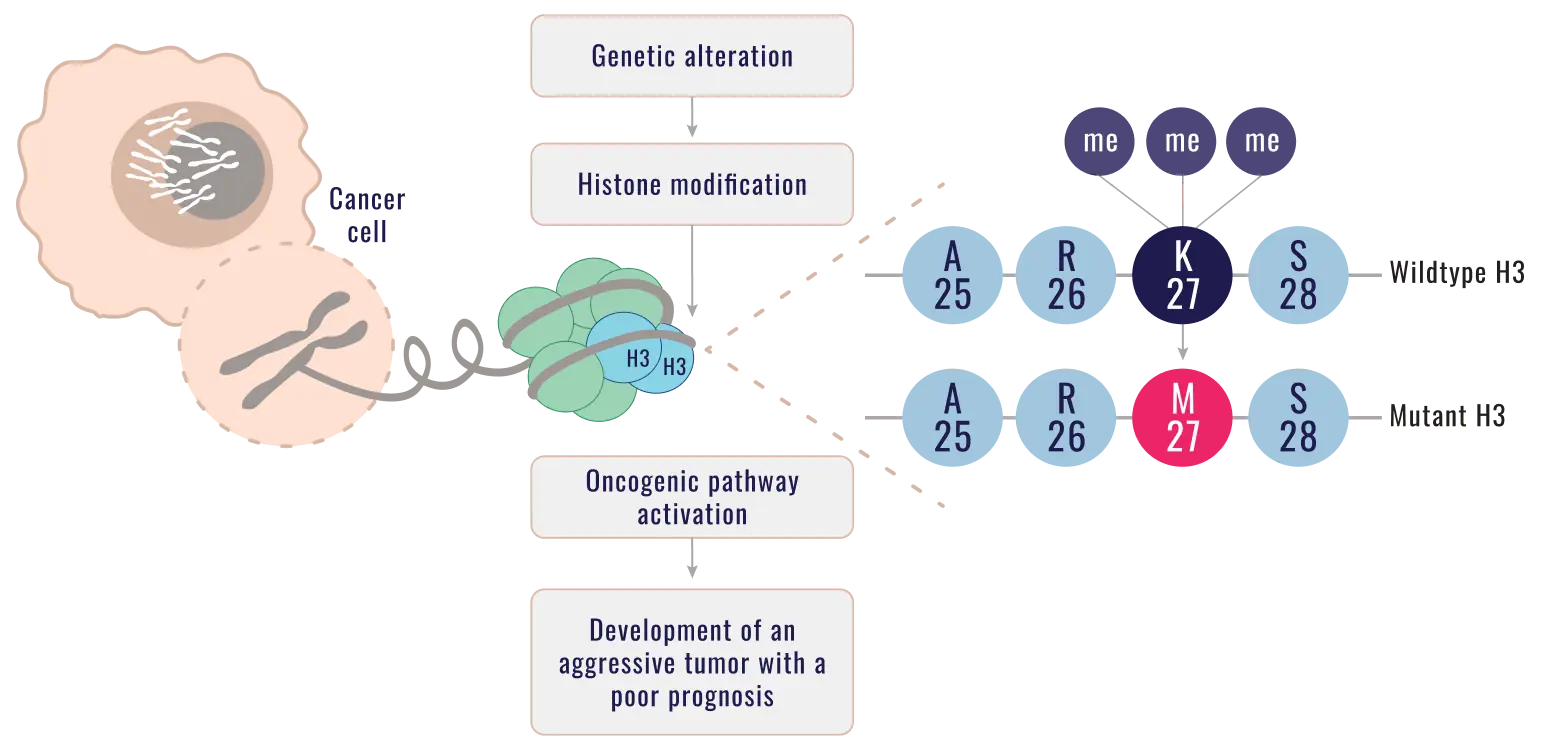
H3 K27me3 loss4,6
- Disrupts epigenetic pathways
- Results in activation of oncogenic pathways
- Leads to a cascade of events that results in diffuse gliomas with a poor prognosis
Prognosis is poor for patients with H3 K27M–mutant diffuse glioma, with a median overall survival of approximately 1 year from diagnosis1-3
The World Health Organization classifies diffuse gliomas with an H3 K27M mutation as Grade 4 irrespective of diffuse glioma histology.4,7,8
The Need for Biopsy
Brain tumor biopsy can unlock crucial insights4,9-11
The decision to biopsy is a critical step when managing gliomas4,9-11
While there is always surgical risk, modern advancements in image-guided stereotactic biopsy have enhanced access to midline tumors and improved biopsy safety.4,9,10
With these improvements, studies of thalamic and brain stem biopsies now show4,9:
of transient neurological damage
of permanent
disability
IHC and NGS Testing
Early molecular testing is essential for proper diagnosis4,12
Make informed disease-management decisions by identifying mutations as soon as possible4,12
Imaging alone cannot confirm mutational status—a biopsy with subsequent immunohistochemistry (IHC) or next-generation sequencing (NGS) reveals specific mutations, such as H3 K27M, that can inform and help optimize disease management.13-15
IHC is widely accessible and highly sensitive for identifying H3 K27 variants as it uses antibodies specific to H3 K27M and H3 K27me313,16,17
NGS can detect a broad range of genomic alterations to identify specific mutations and potential therapeutic targets13,18
Both techniques are standard practice for the accurate diagnosis of gliomas and provide additional data to help tailor treatment plans.4,13,18
Management Methods
Treating H3 K27M–mutant diffuse gliomas is challenging13,19
FAQs
Answers to questions about H3 K27M–mutant diffuse glioma
The H3 K27M mutation results in an alteration of histone H3 function, disrupting normal gene regulation and contributing to activation of oncogenic pathways. Gliomas harboring this mutation are typically aggressive and associated with poor prognosis.4,22
The World Health Organization (WHO) classifies diffuse gliomas with an H3 K27M mutation as Grade 4 (aggressive, spreads rapidly) irrespective of diffuse glioma histology.4,8
An H3 K27M mutation cannot be identified through imaging alone. Diagnosis requires molecular testing of a tumor sample to confirm the presence or absence of a mutation.13-15
Immunohistochemistry or next-generation sequencing can be used to detect the H3 K27M mutation and should be added to routine testing.4,13,16,18
Clinical guidelines recommend early molecular testing of diffuse gliomas for key biomarkers.4,12
Patients with H3 K27M–mutant diffuse glioma are typically given a poor prognosis, with a median overall survival of about 1 year post diagnosis.1-3
H3 K27M–mutant diffuse gliomas can occur across the brain, in both midline and non-midline structures. They should be considered for all patients with diffuse gliomas because identification of specific mutations provides important information to guide medical management.4,5,13,18
Stay Informed
Test every glioma for H3 K27M as early as possible4,12
Identifying an H3 K27M mutation can help inform prognosis and clinical management. Now, with advances in biopsy and molecular testing techniques, identifying mutational status is more achievable than ever before.12,14,15
Get the latest on H3 K27M–mutant diffuse glioma developments
References: 1. Vuong HG, Ngo TNM, Le HT, et al. Prognostic implication of patient age in H3K27M-mutant midline gliomas. Front Oncol. 2022;12:858148. doi:10.3389/fonc.2022.858148 2. Ostrom QT, Shoaf ML, Cioffi G, et al. National-level overall survival patterns for molecularly-defined diffuse glioma types in the United States. Neuro Oncol. 2023;25(4):799-807. doi:10.1093/neuonc/noac198 3. Zheng L, Gong J, Yu T, et al. Diffuse midline gliomas with histone H3 K27M mutation in adults and children: a retrospective series of 164 cases. Am J Surg Pathol. 2022;46(6):863-871. doi:10.1097/PAS.0000000000001897 4. Saratsis AM, Knowles T, Petrovic A, Nazarian J. H3K27M mutant glioma: disease definition and biological underpinnings. Neuro Oncol. 2024;26(suppl 2):S92-S100. doi:10.1093/neuonc/noad164 5. Nakatogawa H, Fukai J, Kawaji H, et al. Characteristics and outcomes of diffuse non-midline gliomas with H3F3A gene mutation in the Kansai Molecular Diagnosis Network for CNS Tumors (Kansai Network): multicenter retrospective cohort study. Acta Neuropathol Commun. 2025;13(1):77. doi:10.1186/s40478-025-01989-y 6. Weinberg DN, Allis CD, Lu C. Oncogenic mechanisms of histone H3 mutations. Cold Spring Harb Perspect Med. 2017;7(1):a026443. doi:10.1101/cshperspect.a026443 7. Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016;131(6):803-820. doi:10.1007/s00401-016-1545-1 8. Louis DN, Perry A, Wesseling P, et al. The 2021 WHO Classification of Tumors of the Central Nervous System: a summary. Neuro Oncol. 2021;23(8):1231-1251. doi:10.1093/neuonc/noab106 9. Sheikh SR, Patel NJ, Recinos VMR. Safety and technical efficacy of pediatric brainstem biopsies: an updated meta-analysis of 1000+ children. World Neurosurg. 2024;189:428-438. doi:10.1016/j.wneu.2024.06.163 10. Kline C, Jain P, Kilburn L, et al. Upfront biology-guided therapy in diffuse intrinsic pontine glioma: therapeutic, molecular, and biomarker outcomes from PNOC003. Clin Cancer Res. 2022;28(18):3965-3978. doi:10.1158/1078-0432.CCR-22-0803 11. Khuong-Quang DA, Buczkowicz P, Rakopoulos P, et al. K27M mutation in histone H3.3 defines clinically and biologically distinct subgroups of pediatric diffuse intrinsic pontine gliomas. Acta Neuropathol. 2012;124(3):439-447. doi:10.1007/s00401-012-0998-0 12. Horbinski C, Solomon DA, Lukas RV, et al. Molecular testing for the World Health Organization classification of central nervous system tumors: a review. JAMA Oncol. 2025;11(3):317-328. doi:10.1001/jamaoncol.2024.5506 13. Vallero SG, Bertero L, Morana G, et al. Pediatric diffuse midline glioma H3K27- altered: a complex clinical and biological landscape behind a neatly defined tumor type. Front Oncol. 2023;12:1082062. doi:10.3389/fonc.2022.1082062 14. Horbinski C, Nabors LB, Portnow J, et al. Central nervous system cancers, version 2.2022: featured updates to the NCCN Guidelines. J Natl Compr Canc Netw. 2023;21(1);12-20. doi:10.6004/jnccn.2023.0002 15. Gajjar A, Mahajan A, Bale T, et al. Pediatric central nervous system cancers, version 2.2025. J Natl Compr Canc Netw. 2025;23(3):113-130. doi:10.6004/jnccn.2025.0012 16. Bechet D, Gielen GGH, Korshunov A, et al. Specific detection of methionine 27 mutation in histone 3 variants (H3K27M) in fixed tissue from high-grade astrocytomas. Acta Neuropathol. 2014;128(5):733-741. doi:10.1007/s00401-014-1337-4 17. Penkova A, Kuziakova O, Gulaia V, et al. Comprehensive clinical assays for molecular diagnostics of gliomas: the current state and future prospects. Front Mol Biosci. 2023;10:1216102. doi:10.3389/fmolb.2023.1216102 18. Kim T, Lee A, Ahn S, Park JS, Jeun SS, Lee YS. Comprehensive molecular genetic analysis in glioma patients by next generation sequencing. Brain Tumor Res Treat. 2024;12(1):23-39. doi:10.14791/btrt.2023.0036 19. van den Bent M, Saratsis AM, Geurts M, Franceschi E. H3 K27M-altered glioma and diffuse intrinsic pontine glioma: semi-systematic review of treatment landscape and future directions. Neuro Oncol. 2024;26(suppl 2):S110-S124. doi:10.1093/neuonc/noad220 20. Karremann M, Gielen GH, Hoffmann M, et al. Diffuse high-grade gliomas with H3 K27M mutations carry a dismal prognosis independent of tumor location. Neuro Oncol. 2018;20(1):123-131. doi:10.1093/neuonc/nox149 21. Ryba A, Özdemir Z, Nissimov N, et al. Insights from a multicenter study on adult H3 K27M-mutated glioma: surgical resection's limited influence on overall survival, ATRX as molecular prognosticator. Neuro Oncol. 2024;26(8):1479-1493. doi:10.1093/neuonc/noae061 22. Louis DN, Giannini C, Capper D, et al. cIMPACT-NOW update 2: diagnostic clarifications for diffuse midline glioma, H3 K27M-mutant and diffuse astrocytoma/anaplastic astrocytoma, IDH-mutant. Acta Neuropathol. 2018;135(4):639-642. doi:10.1007/s00401-018-1826-y